I've been interested in the notion of a Personal Health Record for a long time. I was involved in the development of HotHealth, which launched at the end of 2000, a not-so-auspicious year, given the dot com crash! By the time HotHealth was completed , all the potential competitors identified in the pre-market environmental scan were defunct. It certainly wasn't easy to get any traction for HotHealth take-up and yet only recently it has been retired. For a couple of years it was successfully used at the Royal Children's Hospital, cut down and re-branded as BetterDiabetes to support teenagers self-manage their diabetes and communicate with their clinicians, but it wasn't sustained.
This is not an uncommon story for PHRs. It is somewhat comforting to see that the course of those such HealthVault and GoogleHealth have also not been smooth and fabulously successful :-)
Why is the PHR so hard?
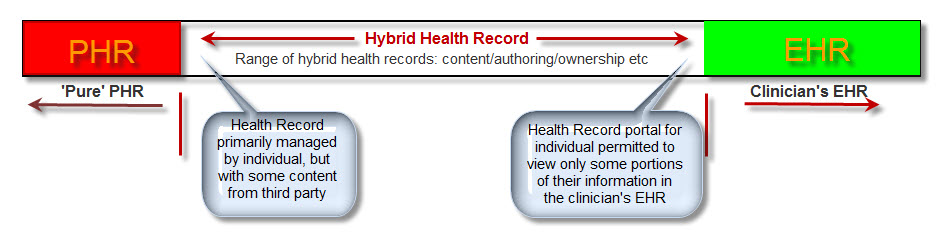
In recent years I participated in the development of the ISO Technical Report 14292:2012: Personal health records -- Definition, scope and context. In this my major contribution seemed to be introducing the idea of a health information continuum.
However in the past year or so, my notion of an ideal PHR has moved on a little further again. It has arisen on the premise of a health record platform in which standardised health information persists independently of any one software application and can be accessed by any compliant applications, whether consumer- or clinician-focused. And the record of health information can be contributed to by any number of compliant systems - whether a clinical system, a PHR or smartphone app. The focus is on the data, the health record itself; not the applications. You will have seen a number of my previous posts, including here & here!
So, in this kind of new health data utopia, imagine if all my weights were automatically uploaded to my Weight app on my smartphone wirelessly each morning. Over time I could graph this and track my BMI etc. Useful stuff, and this can be done now - but only into dead-end silos of data within a given app.
And what if a new fandangled weight management application came along that I liked better - perhaps it provided more support to help me lose weight. And I want to lose weight. So I add the new app to my smartphone and, hey presto, it can immediately access all my previous weights - all because the data structure in both apps is identical. Thus the data can be unambiguously understood and computed upon within the second app without any data manipulation. Pretty cool. No more data silos; no more data loss. Simply delete the first app from the system, and elect to keep the data within my smartphone health record.
And as I add apps that suit my lifestyle, health needs, and fitness goals etc, I'm gradually accumulating important health information that is probably not available anywhere else. And consider that only I actually know what medicines I'm taking, including over the counter and herbals. The notion of a current medication list is really not in the remit of any clinician, but the motivated consumer! And so if I add an app to start to manage my medications or immunisations this data could be also used across in yet another compliant chronic disease support app for my diabetes or asthma or...
I can gradually build up a record of health information that is useful to me to manage my health, and that is also potentially useful to share with my healthcare providers.
Do you see the difference to current PHR systems?
I can choose apps that are 'best of breed' and applicable to my need or interest.
I'm not locked in to any one app, a mega app that contains stuff I don't want and will never use, with all the overheads and lack of flexibility.
I can 'plug & play' apps into my health record, able to change my mind if I find features, a user interface or workflow that I like better.
And yet the data remains ready for future use and potentially for sharing with my healthcare providers, if and when I choose. How cool is that?
Keep in mind that if those data structures were the same as being used by my clinician systems, then there is also potential for me to receive data from my clinicians and incorporate it into my PHR; similarly there is also potential for me to send data to my clinician and give them the choice of incorporating this into their systems - maybe my blood glucose records directly obtained from my glucometer, my weight measurements, etc. Maybe, one day, even MY current medicine list!
In this proposed flexible data environment we are avoiding the 'one size fits all', behemoth approach, which doesn't seem to have worked well in many situations, both clinical systems or personal health records. Best of all the data is preserved in the non-proprietary, shared format - the beginnings of a universal health record or, at least, a health record platform fully supporting data exchange.
What do you think?