The lack of a common health data language has been ‘the elephant in the room’ for a very long time. Unfortunately, very few people acknowledge the need for a clinical lingua franca as a critical foundation for eHealth. The mainstream view seems to be that messages are/will be enough and that creating a standard language for health information is either too hard or too complicated. Is it really that hard? Or is that just the view of those with vested interest in perpetuating the message paradigm?
The 3 C's of health data
Journey to interoperability II
Journey to interoperability I
"Smart data, smarter healthcare"
Case Study: Clinical Engagement
Bridging the gap between the clinical experts and software engineers involved in eHealth projects is well known for being difficult and frustrating for both sides. The openEHR methodology is having great success in bringing the non-technical clinicians along with us on the clinical modelling journey.
Brazilian EHR innovation, powered by openEHR
The Archetype 'Elevator Pitch'
Archetypes in the Real World
I've spent the past week in Ljubljana, Slovenia. Ian McNicoll (@ianmcnicoll) and I were been training clinicians about archetypes and clinical knowledge governance, ready for the launch of their national CKM. A highlight was a side trip to visit the state-of-the-art Paediatric Intensive Care Unit in Ljubljana. The electronic health record has been running there now for two years, with electronic processes gradually taking over. I was escorted by the clinician in charge of the ICU, Professor Kalan. The purpose of the visit – for him to meet someone who facilitated the archetypes used to run his EHR and for me to see our collective international archetype work implemented and used for real clinical purposes, largely under the expert clinical informatics guidance from Ian.

I was thrilled and a little taken aback, all at once. It is one thing to sit in an office researching clinical models and then to remotely collaborate with our international archetype community. But it is another to see real-time data being collected half a world away from home and knowing that we all had a small part in this, especially to support such critical care for a newborn baby. In the photo, above, you might just be able to spot a humidicrib surrounded by all of the equipment.
The majority of these archetypes were built by the international openEHR community for various projects and now utilised under the CC-BY-SA license by the EHR company to develop their clinical system. There are some local archetypes in use as well – added for practical and pragmatic purposes - but these are very much in the minority. These same international archetypes are also being used in the EHR repository in the Northern Territory, Australia, and are underpinning their current work on shared antenatal care and hearing health programs. Soon this work is to be extended for renal failure and heart disease. And across more than 20 sites in Australia we have an infection control system that is using both archetypes and some that have been built specifically to support infection control activities and outbreak management. These shared archetypes are also underpinning work in UK, Brazil, Japan and Sweden.
Next week Ian and I are in Norway to support the Norwegian national archetype effort – training their clinicians and informaticians about archetypes, and especially governance principles at a national level.
There are now 5 CKMs in existence:
- the openEHR international CKM;
- Australia;
- City of Moscow;
- UK clinical community; and the brand new
- Slovenian eHealth program CKM.
The international CKM will continue to gather quality archetypes from all sources and coordinate international review and modelling activities. The intent is for this CKM to be the first port of call for those looking for an archetype.
The national-, organisation- or program-based CKMs will be focussed on supporting local health IT activities and will leverage the international pool of archetypes by a virtual 'read only' reference capability as well as hold specific local archetypes or modifications of the international archetypes that will support local implementation.
Above all the aim is to create high quality, computable, clinical content definitions that have been developed and ratified by the clinicians themselves. In turn this will support collection of good quality data that can be used for a variety of purposes – ranging from the health record itself; through querying and knowledge-based activities such as decision support; aggregation, analysis and research; and secondary use, including population health activities.
I have said it before, but let me say it again…
IT. IS. ALL. ABOUT. THE. DATA.
In the discussions about standards, the standardisation of data is usually missed.
Seeing this little baby in a humidicrib in amongst all of the 'machines that go beep' has invigorated me again.
Let's continue, and even accelerate, our collaboration on the development of archetypes. This will enable us to gather the data we need to provide the kind of healthcare our patients deserve.
Social media and #healthIT
Curious how the majority of #HIT100 nominations are US-based. So much #healthIT talent internationally clearly not using SoMe in same way — Heather Leslie (@omowizard) July 5, 2013
Nominations for the #HIT100 list are in full swing. Well, at least it is full swing in the US. It doesn't seem to be making many waves elsewhere in the twitterverse - a curious phenomenon from my POV.
In the first #HIT100 list (2011), there were definitely 3 (maybe 4 or 5 at most, correct me if I'm wrong) twits/tweeters/tweeple (whatever the correct term is) from outside the US. I remember two from Australia and one from UK. I know because I specifically went looking.
Certainly if you search for health IT-related topics on Twitter or follow some of the health IT related lists, the predominant topics are about US-based activity - Meaningful Use, ONC etc.
If you believe Twitter, then the US is the go-to place for all things health IT. But we know that is not the case. Clearly the use of social media, and specifically Twitter, is vastly different between USA and... well... anywhere else.
I nominated some people to the #HIT100 list this year. Most were non-US-based. My small attempt to try to subvert and upset the balance a little.
It was pleasing to see Keith Boone took a similar view.
I'll be very interested to see how the results of the nominations are presented. If it is truly not a personality or population contest then I would like to see the range of people highlighted, especially with an international focus to broaden the world view and enhance international discourse.
I see evidence of much excellent work happening all around the world related to eHealth, EHRs and health informatics but it is disproportionately represented if you rely on Twitter.
A curious dichotomy.
Even the florists are concerned...
 This tweet from my local florist, only yesterday, speaks for itself.
This tweet from my local florist, only yesterday, speaks for itself.
The White Wizard is Walking
I received my Walking Jacket at the reception desk of my Italian hotel. I'd just paid an exorbitant amount of tax in exchange for receive my jacket from the Italian Postal Service for my trusty, favourite jacket to be turned into a disruptive artwork by @ReginaHolliday. I first wore it to the Medical Informatics Europe Conference in Pisa in August 2012 and then to the ISO TC 215 meeting in Vienna the following September. I'd heard about Regina and her family's story some time before, my awareness raised purely through the twitter community, and then finding images of her 73 cents mural. I finally met her at HIC12, the Australian health informatics conference in Sydney in early August.
Regina was a keynote speaker and during her HIC address, many in the audience were clearly moved. It is the only presentation that I have seen in the health IT environment that received a standing ovation – powerful stuff. It polarised people. Most loved it and felt inspired; some thought it inappropriate in a healthIT conference – go figure!
Regina and I talked one night at dinner. She offered to paint me a jacket. I felt a bit like a fraud – I have no special patient data faux pas story to tell. My involvement in health IT stems from having a long-term engagement with the health system from the tender age of 5; about how that influencing my decision to become a doctor; and my subsequent, almost accidental, slip sideways into health informatics. Nowadays my work focus is firmly on getting health data right, working collaboratively with international clinicians to agree on common definitions about how to represent clinical content in electronic health records.
 And yet here is my jacket – a favourite that I bought way back in 2000 for my first foray out of clinical practice and into the corporate world - my first step into health informatics. I hadn't worn it for a while and Regina's painting has given it a new lease of life. It now has its own story - having travelled to the US to be painted, on to Europe to be worn for the first time in Italy and Vienna, and now back home to Australia.
And yet here is my jacket – a favourite that I bought way back in 2000 for my first foray out of clinical practice and into the corporate world - my first step into health informatics. I hadn't worn it for a while and Regina's painting has given it a new lease of life. It now has its own story - having travelled to the US to be painted, on to Europe to be worn for the first time in Italy and Vienna, and now back home to Australia.
Regina hasn't explained the image to me. I've asked … and waited. She promised to blog about it, but I think I'll be waiting a while. In her gallery of jackets that tell personal stories, mine is number 176.
So let me share what I think it portrays…
I was hit by a car when I was five years old. As a result I started my first day of school on crutches and in plaster from my waist to my right ankle – that young girl on crutches and wearing a caliper is me. Mini-me!
That accident resulted in some permanent problems and I ended up experiencing a series of operations during my childhood and early teenage years. Way too much time was spent in hospital than was healthy, but I still remember telling my orthopaedic surgeon that I wanted to be a Nurse. I remember him saying 'Rubbish. You shouldn't do that much walking. You should be a Doctor, instead"! Maybe it planted a seed. I don't remember it influencing my decision to enter medicine, but that is where I found myself. I'm not sure that as a young intern and resident years we walked less than the nurses – my memory is we never stopped running!
I practiced medicine for over 15 years, gradually side-stepping into health informatics as I joined my husband in developing, marketing, selling, supporting one of the first prescribing systems in Australia. He was the geek GP, passionate to combine his love of clinical practice with technology. I merely agreed to support him in his venture, having absolutely no idea what I was getting myself into.
That kickstarted the health informatics chapter of my life – 17 years duration to date - which has propelled my husband and myself jointly into the world of business, from cottage industry to large corporate consulting firms, and travel to some extraordinary places.
 The adult woman in Regina's image is also me – as the 'omowizard'. This has become my online persona, largely now related to Twitter and blogging. 'omowizard' originated from a love of Tolkien and seeking a Hotmail account back in 2000. Gandalf was taken, as was the 'white wizard'. So given my laundry responsibilities for my young family at the time, I became whiter than white – the Omo wizard. For those unaware, Omo is a brand of clothes washing powder that at the time claimed to wash clothes 'whiter than white'! I never dreamed anyone else would ever have to know or understand that, not even when I experimented on Twitter for the first time as @omowizard. Now it is probably too late to change :)
The adult woman in Regina's image is also me – as the 'omowizard'. This has become my online persona, largely now related to Twitter and blogging. 'omowizard' originated from a love of Tolkien and seeking a Hotmail account back in 2000. Gandalf was taken, as was the 'white wizard'. So given my laundry responsibilities for my young family at the time, I became whiter than white – the Omo wizard. For those unaware, Omo is a brand of clothes washing powder that at the time claimed to wash clothes 'whiter than white'! I never dreamed anyone else would ever have to know or understand that, not even when I experimented on Twitter for the first time as @omowizard. Now it is probably too late to change :)
In the painting I am standing in isolation on a very tall, narrow, bleak pillar. I'm not quite sure what that is representing. Some have suggested a reference to Sauron's tower in Lord of the Rings, but maybe that's too fanciful! I certainly don't have any magic powers. My youngest child informed me recently that I have a strong maternal death stare as a superpower, but I don't think that counts. Maybe it represents the approach that we have been using to standardise the clinical content for health records. It is known as openEHR and although I have been heavily involved in developing the clinical modelling side of it – building archetypes and training others. It has stood in isolation for many years and outside of the mainstream approaches to health IT, but in recent years has become recognised and is gaining increasing recognition as a significant contributor towards the goal of semantic interoperability. Only Regina knows the answer to this one!
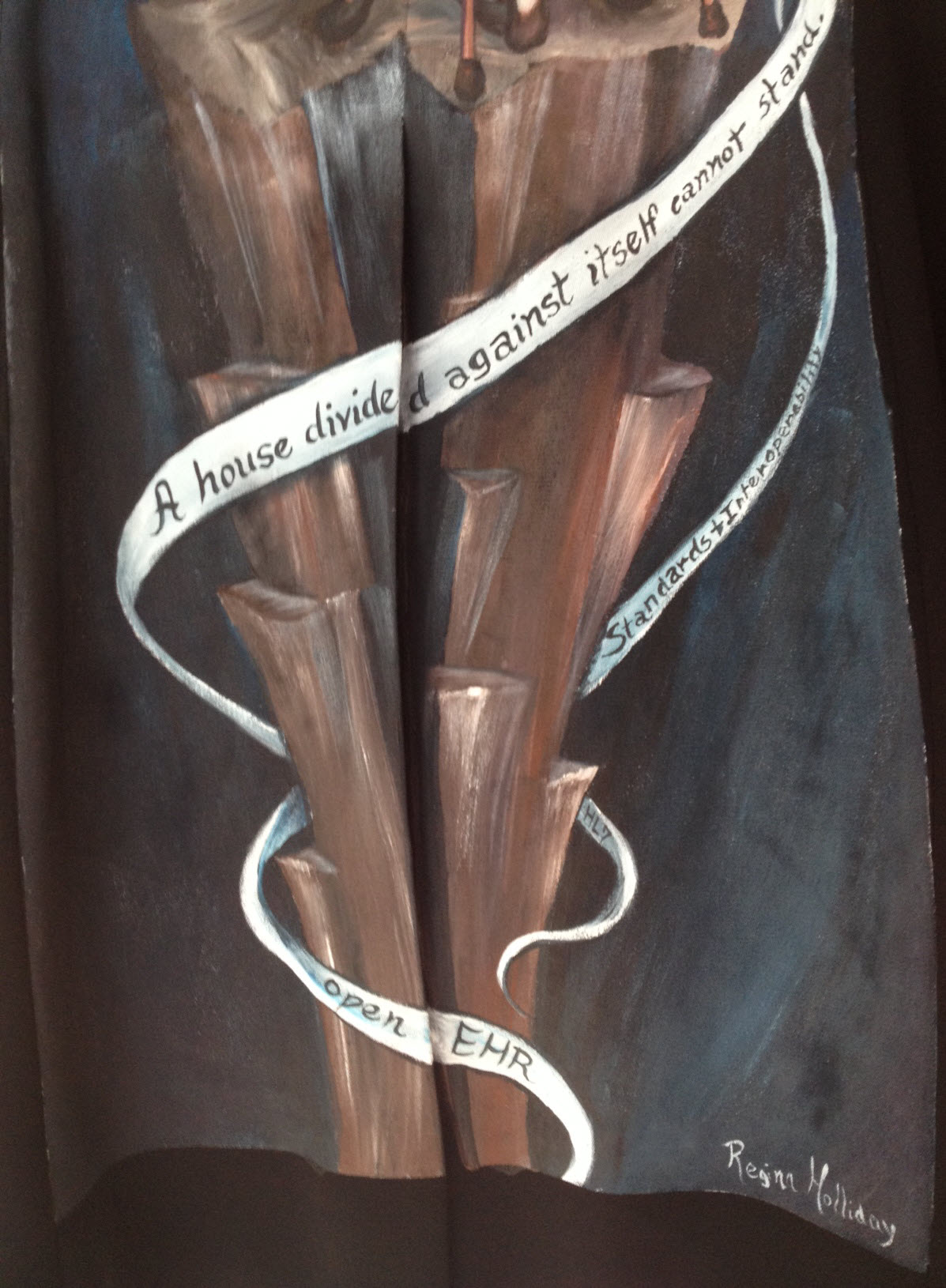 The ribbons or strands entwining around the tower are really interesting to me. The main one rippling across the tower reads: "A house divided against itself cannot stand". This appears to be a direct reference to Jesus' words in Matthew 12:25 – "He knew what they were thinking and told them, "Every kingdom divided against itself is destroyed, and every city or household divided against itself will not stand." (NIV 2012). Abraham Lincoln used the phrase in a speech to Republican candidates at the Republican State Convention on June 16, 1858 relating to the danger of slavery-based disunion. Apparently it is still used sometimes in political speeches, calling for unity and working together for a common goal.
The ribbons or strands entwining around the tower are really interesting to me. The main one rippling across the tower reads: "A house divided against itself cannot stand". This appears to be a direct reference to Jesus' words in Matthew 12:25 – "He knew what they were thinking and told them, "Every kingdom divided against itself is destroyed, and every city or household divided against itself will not stand." (NIV 2012). Abraham Lincoln used the phrase in a speech to Republican candidates at the Republican State Convention on June 16, 1858 relating to the danger of slavery-based disunion. Apparently it is still used sometimes in political speeches, calling for unity and working together for a common goal.
The lowest ribbon says simply, 'openEHR'; the one immediately to its right, 'HL7'; and just above it, 'Standards and Interoperability'.
I had described the approach that we are taking with our openEHR clinical modelling to Regina as one in which we are engaging with clinicians and domain experts to verify that the computable definitions that we are building in openEHR systems are fit for purpose. It is a collaborative approach that is crowdsourcing clinical expertise using the Clinical Knowledge Manager tool. For many years there had been little engagement with the HL7 community as a whole, although recently there appear to have been a softening of the lines of political demarcation. Those not constrained by political blinkers can see there could be significant mutual benefit from openEHR content definitions being used within HL7 constructs. Who knows if this will eventuate? And then there are other opportunities such as the CIMI and FHIR projects… Collaborating is the key.
So I interpret the ribbons yielded by the omowizard as another way of Regina calling for collaboration and collective action in healthIT. It seems that she is portraying me as a coordinator of some of the standardisation occurring in healthIT around the archetype work – using the @omowizard's twitter and blogging being one of the means to coordinate and share the passion, perhaps!
I love the painting but in trying to interpret it, it is not a comfortable image for me. I don't like being the focus. I am certainly enjoying my small bit part in the openEHR clinical modelling and health IT standards world. I have come to openEHR when it was relatively immature. We are seeing it grow and become established, but it is definitely not my idea or vision. I'm just one of number who have had the exciting opportunity of being a facilitator for something that I believe will make a difference.
I hope that when I wear this jacket it will trigger some discussions that might further progress in sharing health information and impacting the provision of health care – that is reason enough to wear it.
Thankyou, Regina. My jacket is a piece of art that is beautiful to look at; It is a powerful statement when understood in context of its origins; and is potentially a disruptive force when considered as part of the larger international Walking Gallery movement. I look forward to more opportunities to wear it at home in Australia and in my travels.
The Times, They Are a-Changin’...
Channelling Bob Dylan? Not quite! But it is interesting to see some emerging HL7 and openEHR activity, at least in this little part of the world – Australia and New Zealand :) Maybe this is a model for the rest of the world - at least food for thought!
For too many long years there appears to have been a palpable barrier between the HL7 and openEHR communities. Some individuals have managed to bridge it, but there has definitely been a reluctance to engage at organisational level. It stems from before my time; I suspect vocal personalities with strong, diverging opinions were at the root. To some, it is a little like a religious argument – where "only my way is the right way"!
Be that as it may - the barrier appears to be softening and became evident to me for the first time back in January last year as I attended the HL7 meeting in Sydney. A full day openEHR workshop was presented by a diverse group of Australian companies plus NEHTA experts; Bob Dolin in attendance, amongst others. Keith Boone tweeted his initial impression of the openEHR approach after I demonstrated our tooling and then blogged about it. My thoughts were captured in my Adventures of a clinician in HL7 post.
Fast forward to 2012…
You may have seen some announcements from New Zealand. Firstly, publication in April of the Health Information Exchange Architecture Building Blocks where they specified "2.3.2 The data definitions of the Content Model shall be formulated as openEHR archetypes" within the "10040.2 HIE Content Model, a framework for the creation of a common set of logical data definitions" document.
And secondly: HL7 New Zealand and the openEHR Foundation signed a Statement of Collaboration - also announced April 2012. Now there's a headline that might have been a surprise to many – HL7 NZ & openEHR clearly intending to work closely together!
Only last Thursday Hugh Leslie & I participated in a seminar, "Bringing the Electronic Health Record to Life," organised by HL7 NZ, Health Informatics New Zealand (HINZ) and the University of Auckland. Prof Ed Hammond, 'the father of HL7', keynoted the meeting: "EHR - The Killer App". In the afternoon mini-tutorials, David Hay presented on FHIR, and Hugh, I and Koray Atalag presented a little about our openEHR work, including clinical knowledge governance and clinician engagement. Koray (a HL7 NZ member and openEHR localisation program coordinator) announced within the meeting that HL7 NZ is the likely organisation to auspice a NZ chapter of openEHR. Now that definitely has to start to change the openEHR/HL7 dynamic somewhat, even if HL7 NZ is a relatively small international affiliate :). The HL7 NZ leadership, to their absolute credit, are certainly not being constrained by any traditional 'turf wars'.
The following day, last Friday, Hugh and I presented a full day workshop on openEHR, again sponsored by HL7 NZ, HINZ and the University of Auckland. As I understand it, this was the first opportunity for the openEHR approach to be socialised with the broader healthIT community in NZ; about 25 in attendance including members of the HL7 NZ Board, vendors, and regional and HealthIT Board reps. The focus was on how openEHR could support the creation of a range of technical artefacts to meet NZ's requirements for CDA messaging (and beyond), generated from a cohesive and governed pool of clinical content models.
Interestingly we had a surprise attendee for the workshop – Ed Hammond joined us for the whole day. I won't presume to guess what Ed has taken away from the day, although he did offer up a comment to the group about the value of exploring use of archetype content directly within CDA.
Post workshop one of the attendees tweeted:
"At #HINZ #openEHR talks last 2 days. openEHR is a fantastic foundation for practical action. Left knowing steps I will take. How cools that!"
And of course, there is an HL7 AU meeting in Sydney early next week entitled "FHIR? CIMI? openEHR? What's the Future of eHealth & mHealth Standards?" The agenda:
- Keynote: Ed Hammond (again) – "FHIR, CIMI and openEHR - What's the Future for eHealth Standards?". [It will be very interesting to hear his opinion after last week's openEHR exposure.]
- Grahame Grieve: "FHIR – What is it? Why has it suddenly become so popular?"
- Hugh Leslie: "Recent developments in openEHR and CDA", and
- I'll be reporting on the CIMI project.
It would be an interesting day to be a fly on the wall! 2 HL7-ers and 2 openEHR-ers addressing an HL7 meeting - all exploring alternatives to the current approaches!
So, keep your eye on the space where HL7 intersects with openEHR – might be some interesting developments.
_______________________
Within the openEHR community, and definitely within Ocean Informatics where I work, we are certainly finding that significant interest is being certainly generated from many sources about the process of using standardised and governed openEHR clinical content as a means to generate range of technical artefacts, including CDA. The New Zealand national interest and activity is evident, as outlined above. And in addition:
- In Australia, NEHTA has piloted the use of clinician-reviewed archetypes from the NEHTA Clinical Knowledge Manager as the start point for generating a number of the PCEHR technical specifications. This work is ongoing and being extended.
- CIMI, the initiative that grew out of HL7 but is now independent, is seeking to develop an internationally agreed approach to clinical modelling and generation of multiple technical outputs. It has already agreed to utilise openEHR ADL 1.5 as its modelling formalism and is using the openEHR Reference Model as the starting point for developing a CIMI Reference Model. We watch this progress with interest.
- And Brazil's national program has recently reconfirmed its intention to commence using openEHR.
Whether the final solution is openEHR or CIMI or even something else, I think that the advent of standardised clinical models as the common starting point for generation of a range of technical outputs is upon us. Ignore it at your peril. And specifically, I would suggest that HL7 International should be considering very seriously how to embrace this new approach.
Sticking with the quasi-gospel theme, maybe it is now a bit more like Curtis Mayfield's "People Get Ready":
People get ready There's a train a-coming You don't need no baggage Just a-get on board
Let's leave our baggage behind, get on the 'train' together to collaborate and create something that transcends any health IT domain turf war! Don't get left behind...
Why the buzz about CIMI?
With the recent public statement from the Clinical Information Modelling Initiative (CIMI) my cynical heart feels a little flutter of excitement. Maybe, just maybe, we are on the brink of a significant disruption in eHealth. Personally I have found that the concept of standardising clinical content to be compelling and hence my choice to become involved in development of archetypes. During my openEHR journey over the past 5 or so years it has been very interesting to watch the changing attitudes internationally - from curiosity and 'odd one out' through to "well, maybe there's something in this after all".
And now we have the CIMI announcement...
So what has been achieved? What should we celebrate and why?
At worst, we have had a line drawn in the sand: a prominent group of thought leaders in the international health informatics domain have gathered and, through a somewhat feisty process, recognised that a collaborative approach to the development of a single logical clinical content representation (the CIMI core reference model) is a desirable basis for interoperability across formalisms. Despite most of the participants having significant investment and loyalty to their own current methodology and flavor of clinical models, they have cast aside the usual 'not invented here' shackle and identified a common approach to an initial modelling formalism from which other models will be derived or developed. Whether any common clinical content models are eventually built or not, naming of ADL 1.5 and the openEHR constraint model as the initial formalism is a significant recognition of the longstanding work of the openEHR Foundation team - the early specifications emerged nearly 20 years ago.
At its idealistic best, it potentially opens up a new chapter for health informatics, one that deviates from the relatively safe path of incremental innovation that we have followed for so many years - the reliance on messages/documents/hubs to enable us to exchange health information. There is an opportunity to take a divergent path, a potentially transformational innovation, where the focus is on the data itself, and the message/document/EHR becomes more simply just the receptacle or vehicle for the data. It could give us a very real opportunity to store lifelong health information; simplify data exchange (whether by messages or documents), aggregation, querying and analysis; and support knowledge-based activities such as decision support - all because we will (hopefully) have non-proprietary, common, agreed and fully defined models of clinical content and known transformations between each formalism.
Progress during the next few months will be telling. In January 2012, immediately before the next HL7 meeting in San Antonio, the group will gather again to discuss next steps.
There is a very real risk that despite best intentions all of this will fade away to nothing. The list of participating organisations, including high profile standards organisations and national eHealth programs, is a veritable Who's Who of international health IT royalty, so they will all come with their own (organisational and individual) work experience, existing modelling resources, hope, enthusiasm, cynicism, political agendas, bias and alliances. It could be enough to sink the work of this fledgling group.
But many are battle-weary, having been trudging down this eHealth path for a long time - some now gradually realising that the glacial incremental innovation is not delivering the long-term sustainable answers required for creating 21st Century EHRs as they had once hoped. So maybe this could be the trigger to make CIMI fly!
I think that CIMI is a very bright spark on the health IT horizon. Let's hope that with the right management and governance it can be agilely nurtured into a major positive force for change. And in the future, when its governance is mature and processes robust, we can integrate CIMI into the formal standards processes.
Best of luck, CIMI. We're watching!
The health information continuum
The final draft version of ISO 251's Technical Report "Personal Health Records — Definition, Scope and Context" has just been sent for formal publication. I was involved in some of the later drafting, especially proposing the notion of a spectrum, or continuum of person-centric health records was. The latest iteration, here:
Healthcare organisations and healthcare systems are accountable for the content of EHRs that they control. Individuals have autonomy over records they choose to keep. However, in between these two strict views of an EHR and a PHR is a continuum of person-centric health records which may have varying degrees of information sharing and/or shared control, access and participation by the individual and their healthcare professionals. Toward the EHR end of the spectrum, some EHRs provide viewing access or annotation by the individual to some or all of the clinician’s EHR notes. Towards the PHR end of the spectrum some PHRs enable individuals to allow varying degrees of participation by authorised clinicians to their health information – from simple viewing of data through to write access to part or all of the PHR.In the middle of this continuum there exist a growing plethora of person-centric health records that operate under collaborative models, combining content from individuals and healthcare professionals under agreed terms and conditions depending on the purpose of the health record. Control of the record may be shared, or parts controlled primarily by either the individual or the healthcare professional with specified permissions being granted to the other party.
And the final diagram:
 Australia's PCEHR is an evolving example of a person-centric health record aiming for that somewhat scary middle zone of shared responsibility and mixed governance - carrying with it enormous potential for changing the delivery of healthcare and surmounting enormous clinical, technical, cultural and social challenges.
Australia's PCEHR is an evolving example of a person-centric health record aiming for that somewhat scary middle zone of shared responsibility and mixed governance - carrying with it enormous potential for changing the delivery of healthcare and surmounting enormous clinical, technical, cultural and social challenges.
What kind of things should we be considering?
How can we make the PCEHR a successful and vital component of modern healthcare delivery? What features and attributes will ensure that we steer clear of the approaches of previous failed projects and, instead, create some positive traction?
I've considered these issues for many years as I've watched the PHR/EHR domain wax and wane and I keep returning to 3 major factors that need to be considered from both the consumer and the clinician points of view:
- Health is personal
- Health is social
- Liquid data
These are the big brush stroke items that need to be front and centre when we are designing person-centric health records. Will post some more thoughts soon.
PCEHR insights
Chris Pearce posted this to a closed email list yesterday. I think it provides a useful insight into plans for the Australian Personally Controlled Electronic Health Record (PCEHR) that is not otherwise obvious. The Documents he refers to are two NEHTA specifications that are being developed in consultation with professional bodies, related to the PCEHR Shared Health Summary and PCEHR Event Summary. With his permission:
An overview that you might find helpful in making a bit more sense of the documents. If you need more detail, you may need to go back to the concept of operations document.
The Shared Health Summary (SHS) intended to be a curated, validated record. Initially it was meant to come from general practice, but in the consultation process this has been modified - and is now the role of a 'nominated provider', who must be a health professional who is capable of understanding the continuing, comprehensive care aspect, medications and the like. It will require a mutual consent process.
The event summary was initially designed to pick up where the SHS (which is fixed at a point of time) left off - so if you had something that would alter the SHS, you could put it in the Event summary - so for example- GP loads SHS, then refers patient to specialist who diagnoses diabetes - so loads event summary with diagnosis of diabetes, Rx of metformin. The actual scope is part of the consultation process that ACHI is now involved in.
The third piece of the puzzle is a thing called the consolidated view - which is designed to bring the information together in a meaningful way - SHS, event summaries, discharge summaries, other clinical documents. Thus in the above example a third party would see a list of the current conditions that would include the ones from the SHS (clearly identified as to provenance) along with the ones from an event summary (and from consumer entered data.
But, it does mean that one can have a health summary (uncurated, or really curated at a different level) 'view' built up over time without the shared health summary.
Author: Associate Professor Christopher Pearce PhD MFM MBBS FRACGP FACRRM FAICD FACHI Director of Research, Melbourne East General Practice Network Adjunct Associate Professor in General Practice, Monash University Visiting Fellow, Australian National University Clinical Lead, National E-Health Transitional Authority
Power drills, Cardiologists and collaborative consumption
This week I watched Rachel Botsman's TEDxSydney talk: Collaborative Consumption. Rachel's premise is that we're "wired to share", and I particularly liked her illustration at the 10 minute, 30 second mark... ASSUMPTION #1: Most people own a power drill.
ASSUMPTION #2: Most power drills are used for a total of 12-13 minutes in their entire lifetime << seems not unreasonable.
NEED: We actually need a hole, not a drill!
CONCLUSION: Either rent a drill from someone else, or rent yours to everybody else.
WHAT IS THE END GOAL?: Share the resources better!
[ted id=1037]
While visiting Brazil last year , I learned that in São Paulo if you get referred to a Cardiologist, you don't get to choose which one, you just get sent to one. That doesn't sit well with me, especially as a clinician, and I'm pretty careful to whom I entrust my care, or my family's care.
Yet apparently the waiting time is down to trivial time frames. People are actually getting treated. That is significant!
Apparently resources are being used better, simply because of a central booking system and an algorithm matching clinician with patient and location.
When you start to add in some of the benefits from eHealth such as potential shared EHRs, this starts to make more sense. I will still struggle with the lack of choice, but if patients are being seen more efficiently... then maybe it is a good, or even better, thing.
Stop for a moment and consider:
If we want health reform...
If we want more efficient use of resources for our health $$$...
... then we need to think of how to better use Health IT to support the notion of collaborative health consumption - both of resources & information. How can we better match available resources with need? How can we enable consumer choice at the same time?
There's a tension there - I can foresee many issues, but also opportunities.
I have more questions than answers.
Very interested in your opinion.
Gimme an… uhr?
 What do we have?
You can have all the messages, connect-a-thons and profiles that you like - certainly you will achieve short- to medium-term connectivity wins but it is not enough. It is not sustainable and clinicians want and need to share relevant data when it is needed. Predetermined messages and documents will be a great start, but it's not enough.
What do we have?
You can have all the messages, connect-a-thons and profiles that you like - certainly you will achieve short- to medium-term connectivity wins but it is not enough. It is not sustainable and clinicians want and need to share relevant data when it is needed. Predetermined messages and documents will be a great start, but it's not enough.
You can invest huge resources in terminology - we definitely need it - but terminology in isolation is also not enough.
You can demand all the 'damn data' that you want, but non-standardised data will still largely not be computable - largely limited to read-only access.
What do we want?
We hear talk about:
- shared electronic health records;
- semantic interoperability; and
- health data liquidity.
Essentially these phrases describe different aspects of the same 'elephant in the room'; just using different jargon...
We expect our healthcare professionals to be able to safely exchange important health information. To have the right health information available at the right place at the right time. To prevent us repeating our health histories ad nauseum. In fact a huge percentage of patients assume that we can already do this! But we can't... yet. Shared health records are not easy.
What do we need?
A single data-driven "universal health record", an uhr! And please note the deliberate lack of capitals.
What on earth is an uhr, I hear you quite reasonably ask...? A uhr is simply a non-proprietary pool of standardised health data which can be used for any purpose we want - PHR, EHR, EMR, SEHR, IEHR, research, epidemiology, reporting & stats, shared care, clinical decision support & more. There is no particular EHR application associated with it; in fact it works with any and every software program, vendor and healthcare provider.
The key (and I say it yet again)... it's. all. about. the. data.
In addition, and supported by:
- Collaboration at international, national, jurisdictional or organisation level to share and re-use the clinical data definitions, so that our health information can similarly be shared.
- Clinicians driving the clinical content definitions - reflecting the information they need for recording health care for themselves and their patients, ensuring that EHRs are 'fit for purpose'. Terminology integrated with these structured clinical content definitions to unambiguously define the building blocks of the health record.
As a result:
- Message structures required for data exchange become more about the wrapper and less about content - much easier to negotiate and maintain.
- Vendors no longer have clinicians locked-in to proprietary data silos
- Tools used to do 'clever stuff' with our data need only to be built once to conform to these agreed clinical data definitions - think decision support, reporting, data repositories, and integration. Now that takes away a lot of the barriers we strive to overcome!
- Data in a common format can be exchanged between systems - data liquidity becomes a reality, flowing to where it is needed and according to authorisation and access permissions.
Gimme a universal health record. Gimme my damn, um,... uhr, and let my data flow...
And so, I archetype;-)
What if... grassroots professional clinical colleges were driving EHRs?
Is the tail wagging the dog? Should vendors decide what clinicians need? OR should the professional clinical colleges be driving the EHRs that members need to provide quality healthcare to their patients? From a quality point of view, one could strongly suggest that colleges should be the experts driving this new paradigm of clinical care. As a group, professional clinical colleges as a group usually state that one of their major roles is in establishing and driving the benchmarks for acceptable clinical practice standards in their field of expertise. Most do this very well in the traditional areas of clinical practice.
Scouring the web it is possible to see that some are engaging actively in eHealth. For example, from the website of The Council of the Royal College of Physicians in UK, a vision statement published in January 2010 incorporates this final paragraph:
"Effective implementation of standardised, structured, patient focused records requires strongly led culture change, embraced by all medical and clinical staff. They are essential prerequisites for safe, high quality care and for the safe, efficient and effective migration from paper to electronic patient records. Such records will also enable innovative development of services that cross traditional boundaries and, by giving patients access to their record, empower them to take more responsibility for their own care."
If colleges have had a traditional role in ensuring safe, high quality care, then the advent of electronic health information should logically trigger a natural extension of their pre-existing work and roles into the eHealth arena. I would go further and suggest that they should also be actively driving an eHealth agenda that reflects their college remit regarding provision of quality care and standards; ensuring that the data created, stored, shared and queried is good and fit for use in clinical care.
This agenda may, or may not, be aligned with the activities of national eHealth programs. As we look at the news in recent weeks it is becoming apparent that many are struggling with implementation of top-down agendas. We have seen major changes in the national approach to eHealth happening in Netherlands, Germany, and England's NHS. Perhaps it is time for a grassroots, bottom-up approach from the end-users, the healthcare providers, and their patients, the healthcare consumers.
How can colleges drive eHealth?
- Promote the establishment of a universal health record - a long-term, data-driven health record platform based upon open source specifications, a standardised health data structure, and application-independence. If we place the patient's universal health record at the focus, applications can effectively 'plug & play' with an open, standardised patient data repository, instead of struggling/battling to move/transform/migrate/map/message bits of health information between proprietary application silos.
- Develop clinical quality-related eHealth standards:
- Knowledge artefacts specifications The clinical knowledge expertise of colleges can be used not only to develop principles of best practice and clinical guidelines etc but also the structured clinical content specifications that underpin the universal health record and ensure that the health record is able to capture all the data that their clinicians need to provide quality clinical care, to share with other healthcare professionals and for research. These specifications need to be defined both at the clinical concept level, such as the specification for blood pressure, but also expressing how many clinical concepts can be aggregated together and constrained to specify the requirements for a computable discharge summary or an anaesthetic record. Ideally this would be work done in collaboration with other clinicians, colleges and informaticians to make sure that the agreed concept specifications are applicable for all colleges and clinical domains, so that there is one common concept in use for all. Colleges as domain experts are also best placed to determine the terminology subsets that are appropriate for use by their clinicians.
- EHR best practice: Develop principles around the best practice use of electronic health records, including:
- Data quality principles and activities. As health records become electronic, the previous remit of Colleges to make sure that clinical practices are accredited and that paper records are kept to a documented standard can be transformed to the eHealth paradigm. There are similar principles that can be developed and applied when clinicians are capturing and using data. Programs such as Primus Plus in the UK have worked directly with primary care clinicians to educate and support about best practice data management.
- EHR safety - User interfaces,clinical processes, decision support etc
Colleges may bundle these new standards-based eHealth activities within existing service provision to, or activities involving, their members.
In addition, commercially savvy colleges could develop ways to develop and sell practical solutions or packages around these quality principles direct to members – products or programs to make it easy for members to put the evidence-based and quality principles into practice.
Herein lies a challenge for contemporary professional clinical colleges – to both embrace eHealth and to actively drive it in a way that promotes and preserves safety, quality and best practice in healthcare, such that eHealth becomes a positive tool for healthcare provision and, possibly even, reform.
And how to do this in practice? Well, it is no secret that I think openEHR can offer a solution to a lot of these issues - see my previous posts 'What on earth is openEHR' and 'Connect with openEHR'.
Time will tell if I'm on the right track. For me as a clinician, the more time I spend with it, the more compelling this openEHR story becomes...
Control of the PHR
 Pondering my last post further...
While our reality is that there are both individual- and clinician-focused PHRs, in any PHR where there is co-located content (i.e. of both individual- and healthcare provider-origins) there needs to be a final, single arbiter of content, quality and control. While the ideal is that this should be as shared and collaborative as possible, my personal feeling is that in the long term, successful PHRs will be those with the individual at the helm, with the clinician/s participating as a key partner.
Pondering my last post further...
While our reality is that there are both individual- and clinician-focused PHRs, in any PHR where there is co-located content (i.e. of both individual- and healthcare provider-origins) there needs to be a final, single arbiter of content, quality and control. While the ideal is that this should be as shared and collaborative as possible, my personal feeling is that in the long term, successful PHRs will be those with the individual at the helm, with the clinician/s participating as a key partner.
In addition, a PHR controlled by an individual is more likely to succeed and be used by healthcare providers if there are sound data management processes underlying the PHR to support sound data stewardship for all participants. We can't underestimate the importance of ensuring that provenance of data is transparent, and that contributions to the PHR from external sources such as laboratory reports or discharge summaries remain intact and unedited etc. This is not a technical problem, but requires intelligent PHR design. Both individuals and healthcare providers need to be comfortable with how the individual's data is managed and represented, ensuring protection of the integrity and traceability of externally sourced data, and allowing the individual to annotate or tag data with their own comments or concerns.
Provision of healthcare has traditionally been quite a paternalistic process. We clinicians have acted as stewards on behalf of our patients. Interestingly in my discussions with consumers even in recent years, many are happy for this status quo to continue, not feeling confident or competent to control or manage their health information. Yet ironically these are the same people who operate their own financial affairs, bank online, shop online, email, tweet and blog. Transitioning the control of health information back to the individual may not be as easy as we anticipate. Most groups anticipate that the consumer will be willing to take over as soon as we make their health information available to them. I think that the reality might be more challenging and not without controversy. It will require education processes to support the transition for both the individual and the healthcare provider.
We can pull out that old chestnut and as clinicians declare that data in a health record can't be relied upon unless it has been entered by a clinician, however once you look at any amount of EHR data you will realise that clinician-entered data is not necessarily synonymous with quality. In counterpoint there are an increasing number of clinicians who can tell stories where their patients were able to correct their data when viewing a share computer monitory in a consultation.
I will vote optimistically and promote the case for individual's to control their PHRs. Individuals are best positioned to act as the central integrator for the broadest range of healthcare providers who participate in their care, and I view the adding their own data as a bonus. The broader, the deeper, the richer an individual's health information is, potentially the better the care that can be provided for them.
The sum is greater than the (isolated EHR) parts, let's not undervalue that – encourage individual-controlled PHRs, but always with sound data stewardship as the highest priority.


