Discussion about how to represent some of the commonest clinical concepts in an electronic health record or message has been raging for years. There has been no clear consensus. One of those tricky ones - so ubiquitous that everyone wants to have an opinion - is how to create a computable specification for an adverse reaction.
In the past few years I have been involved in much research and many discussions with colleagues around the world about how to represent an adverse reaction in a detailed clinical model. I'd like to share some of these learnings...
Discussion about how to represent some of the commonest clinical concepts in an electronic health record or message has been raging for years. There has been no clear consensus. One of those tricky ones - so ubiquitous that everyone wants to have an opinion - is how to create a computable specification for an adverse reaction.
In the past few years I have been involved in much research and many discussions with colleagues around the world about how to represent an adverse reaction in a detailed clinical model. I'd like to share some of these learnings...
Making sense of 'Severity'
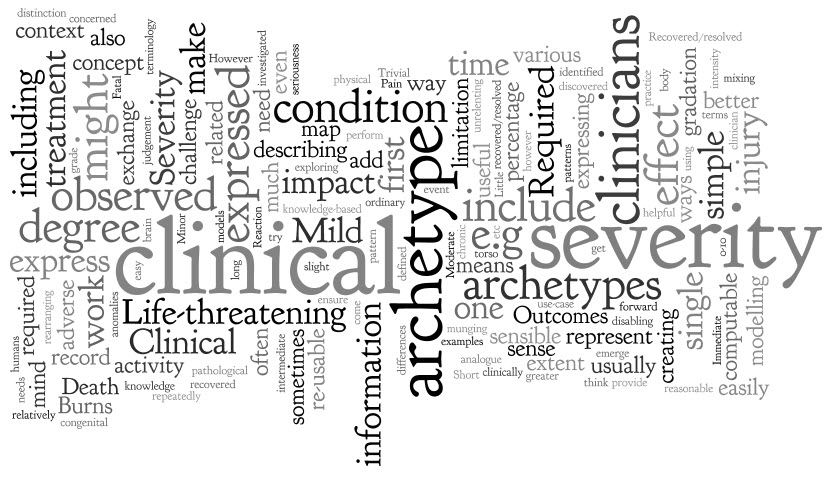 'Severity' is a pretty simple clinical concept, isn't it?
I thought so too until I first sat down to create a single, re-usable archetype to represent 'Severity'. I soon discovered that I had significantly underestimated it - the challenge was greater than appeared at first glance.
'Severity' is a pretty simple clinical concept, isn't it?
I thought so too until I first sat down to create a single, re-usable archetype to represent 'Severity'. I soon discovered that I had significantly underestimated it - the challenge was greater than appeared at first glance.
The archetype development process is usually relatively straight forward - a brain dump of all related information into a mind map, followed by rearranging the mind map until sensible patterns emerge. They usually do, but not this time.
However, the more I investigated and researched, the more I could see that clinicians express severity in a variety of ways, sometimes mixing and 'munging' various concepts together in such a way that humans can easily make sense of it, but it is much harder to represent in a way that is both clinically sensible and computable.
The simple trio of 'Mild', 'Moderate' and 'Severe' is commonly used as a gradation to express the severity of a condition, injury or adverse event. Occasionally these are defined for a given condition or injury, however most often these are subjective and there should be concern that one clinician's mild might be another's moderate. Some also include intermediate terms, such as 'Mild-to-moderate' and 'Moderate-to-severe', but one has to begin to be concerned if these more subtle differences make the judgement even more unreliable, especially if we need to exchange information between systems.
Others add 'Trivial' – is this less than 'Mild'? By how much? Is there a true gradation here? And what of 'Extreme'? Still others add 'Life-threatening' and 'Death' – but are these really expressing severity? Or are they expressing clinical impact or even an outcome?
When exploring severity I found examples of severity expressed by clinicians in many ways. This list is by no means exhaustive:
- Pain – expressed as intensity, often including a visual analogue scale as a means to record it ie rate from 0-10
- Burns – describing percentage of body involved e.g. >80% burns
- Burns – describing the depth of burn by degree e.g. first degree
- Perineal tears – describe the extent and damage by degree – e.g. second degree tear
- Facial tic – expressed in using frequency e.g. occasional through to unrelenting
- Cancer – expressed as a grade, clinical or pathological
- Rash – extent or percentage of a limb or torso covered.
- Minor or major
- Mild, disabling life-threatening
- Relative severity – better, worse etc
- Functional impact – ordinary activity, slight limitation, marked limitation, inability to perform any physical activity
- Short or long term persistence
- Acute or chronic
In practice, clinicians can work interchangeably with any of these expressions and make reasonable clinical sense of it. The challenge when creating archetypes, and other computable models, is to ensure that clinicians can express what they need in a health record, exchange that information safely with other clinicians, allow for knowledge-based activities such as decision support.
In addition, there also needs to be a clear distinction between 'severity' and other, related qualifiers that provide additional context about 'seriousness' of the condition, injury or adverse reaction. These sometimes get thrown into the mix as well, including:
- Clinical impact (or significance);
- Clinical treatment required; and
- Outcomes.
Clinical impact/significance might include:
- None - No clinical effect observed
- Insignificant - Little noticeable clinical effect observed.
- Significant - Obvious clinical effect observed
- Life-threatening - Life-threatening effect observed
- Death – Individual died.
Immediate clinical treatment required might include:
- No treatment
- Required clinician consultation
- Required hospitalisation
- Required Intensive Care Unit
Outcomes might include:
- Recovered/resolved
- Recovering/resolving
- Not recovered/resolved
-
Fatal
Then there are those that recovered or the condition resolved but there were other sequelae such as congenital anomalies in an unborn child...
Severity ain't simple.
Over time, and repeatedly returning to it when modelling it in various archetypes including Adverse Reaction and Problem/Diagnosis, I've come to the conclusion that I don't think it is useful or helpful for us to model 'severity' in a single, re-usable archetype. It seems to work better as a single qualifier element within archetypes – then we can bind it in to terminology value sets that are useful for that specific archetype concept and for the use-case context.
When a clinical knowledge pattern is easily identified, creating an archetype is easy - the archetype almost writes itself! So over time I've learned not to try to force the modelling. Some archetypes 'work'; some, like this one, just don't.
Anatomy of an archetype
 With this blog I want to establish a simple baseline statement or overview about openEHR archetypes, aggregated from other posts and publications – a reference point if you like – from which we can journey further and in more detail into the issues around clinical modelling using specific archetypes.
Archetypes are a strong basis for data liquidity. Create the archetype once, agree through peer-review, re-use when and where required – the foundation for a 'universal health record'.
With this blog I want to establish a simple baseline statement or overview about openEHR archetypes, aggregated from other posts and publications – a reference point if you like – from which we can journey further and in more detail into the issues around clinical modelling using specific archetypes.
Archetypes are a strong basis for data liquidity. Create the archetype once, agree through peer-review, re-use when and where required – the foundation for a 'universal health record'.
Definition:
Formal Definition
An archetype is a computable expression of a domain content model in the form of structured constraint statements, based on a reference (information) model. openEHR archetypes are based on the openEHR reference model. Archetypes are all expressed in the same formalism. In general, they are defined for wide re-use, however, they can be specialized to include local particularities. They can accommodate any number of natural languages and terminologies. [Archetype Definitions and Principles]
Clinician's 'lay' definition:
An archetype is a structured, computable specification for one single, discrete clinical concept. - much simpler!
Each archetype is a rich health data specification, defined and agreed by the clinicians themselves to ensure that each model is 'fit for clinical purpose'. Collectively these archetypes together can create an electronic health record 'lingua franca', or an example of PCAST report's 'Universal Exchange Language (although archetypes are not limited only to exchange of health information).
Archetypes can be used to model a range of clinical concepts:
- Simple and straightforward - such as 'Blood Pressure'; 'Body Weight'; or 'Symptom'; or
- Complex, compound concepts - such as 'Medication order', or recording how a 'Procedure' has been carried out.
Purpose
Archetypes are:
- Potential 'agents for change' – allowing knowledge-driven EHRs as an orthogonal approach to EHR development.
-
The basis for a coherent and consistent approach for the whole continuum of clinical care and related activities:
- Recording, storing and querying health information in electronic health information;
- Exchanging health information - the broader the agreement & governance, the greater the potential for interoperability;
- Data aggregation;
- Knowledge-based activities; and
- Comparative data analysis.
Using archetypes requires:
- A change of mindset – no longer silos of data; no longer message and document driven.
- Upfront planning & coordination in development of archetypes, but not necessarily more time
-
CLINICIAN LEADERSHIP & ENGAGEMENT
- To ensure the quality of clinical data in our EHRs
- To warrant the clinical data is safe & 'fit for purpose'
Design
Each archetype is designed:
- As a maximal data set effectively everything one can think of about a clinical concept in all situations by the consumer and any and all providers. This design intent is pragmatically constrained to be sensible in some situations, however good archetype design will always ensure that the full model can be achieved through nesting of additional archetypes to create the maximal dataset/universal use-case ideal.
- For the 'universal use-case' – for re-use in any and all scenarios, from use at home, to primary care, community care, hospital care, secondary use and for research.
Each archetype needs to represent the variety of data that is required to represent the information required for all aspects of clinical care and related activities, including:
- The ability to capture both free-text vs structured data;
- Normal statements such as "Nil significant" or "NAD";
- Graphable data;
- Images – eg a homunculus, or a surgical diagram;
- Multimedia including photos, video and audio or an ECG wave format;
- Questionnaires, checklists etc
Think about how the clinician may record the data: different clinicians will need differing approaches to recording their health information and the models need to allow for this clinical diversity. Some will prefer to use more free text and others more structure; some need more detail than others; we need to capture current requirements for recording and exchange while keeping in mind what might be best practice in the near and distant future.
The best designers, without a doubt, have a clinical background. I have seen clinicians and non-clinicians given identical clinical content, but the archetypes produces are surprisingly different. Clinician modellers definitely model their domain better than those who are not familiar with clinical practice. They are perhaps better able to envision the fractal nature of medicine and take that in to account in creating archetypes, especially the complex areas which require nesting of archetypes within each other to capture the depth and richness required in the models.
Integration with terminologies such as SNOMED, ICD or LOINC are strategic and important – the structure of an archetype is not enough to represent clinical information adequately, and similarly terminology alone is inadequate. However the combination of terminology within an archetype structure, by naming elements or provision of value sets, is semantically very powerful. There is still considerable work to be done to determine how to represent the information overlap – that which can be expressed either in the archetype structure itself or via terminology. This remains a 'grey zone' and is a pressing area for collaboration or research.
Archetype classes – support clinician's processes
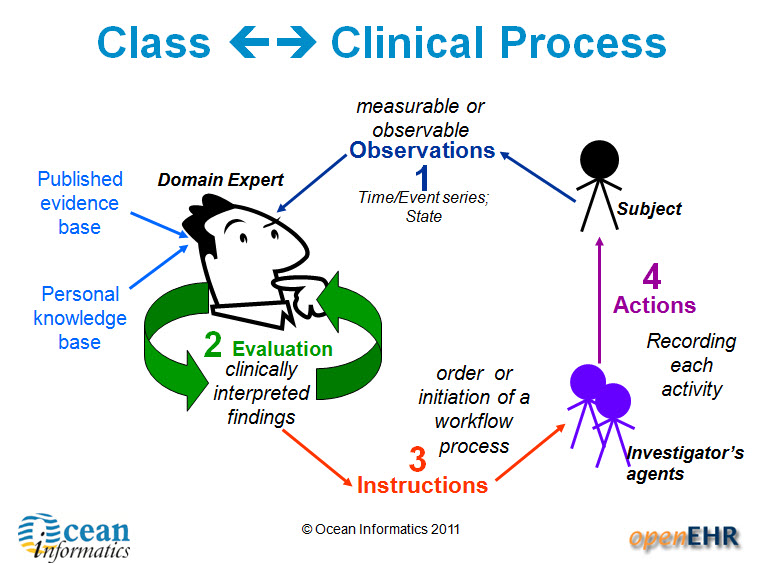
There are four main categories of archetypes that are useful to understand – each corresponding to classes in the openEHR Reference Model.
1. Compositions – which correspond to commonly used clinical documents, such as 'antenatal visit' or 'care plan'. 2. Sections – these are effectively used to assist with human navigation within EHRs and correspond to document headings, for example 'antenatal examination' or 'summary'.
3. Entries – these are the most common and are fundamental building blocks of EHRs. There are four main types of Entry archetypes:
- Observations – recording measurable or observable data e.g. blood pressure, symptoms or weight;
- Evaluations – recording clinically interpreted findings e.g. adverse event, diagnosis or assessment of risk;
- Instructions – recording the initiation of a workflow process, such as a medication order or referral;
- Actions – recording clinical activities e.g. procedure or medication administration. Actions complement the instruction and can record the ensuing state of the instruction, such as 'completed' or 'cancelled'.
4. Clusters
Lifecycle & Governance
The Clinical Knowledge Manager (CKM) – www.openEHR.org/knowledge - is an international, online clinical knowledge repository under the auspice of the openEHR Foundation that provides:
- Access to a library of cohesive archetypes and related knowledge artefacts;
- Peer review, life cycle management & publication process via a Web 2.0 approach for clinical content, terminology binding, terminology reference set binding and translations;
-
Clinical Knowledge governance underpinned by a digital asset management system and providing:
- Provenance, audit trails, validation checking
- Release sets for implementation
Archetypes are freely available under a Creative Commons license.
Use
The need for EHRs to be able to represent clinical diversity is absolutely underrated. Existing EHR systems corral clinicians into certain types of recording etc, but for safety we need more diverse ways for clinicians to record what they need for patient care, and also to ensure that what is exchanged is appropriate for the patient and their individual circumstances. A 'one size fits all' document approach to emergency summaries or messages can be potentially unsafe. Elderly, pregnancy, chronic disease, paediatrics are extremely common examples where there are specific additional requirements needed to summary data sets
Templates are computable specifications for a specific clinical scenario or use-case. The openEHR paradigm takes the governed and agreed archetypes from CKM and creates clinically useful specifications that can be implemented in systems by:
- Aggregating the necessary archetypes together; and
- Constraining the maximal dataset archetypes so that only relevant data elements are active.
Examples include all clinical content required for a specific Message, Document, Clinical consultation or Report e.g. a histopathology report, a referral, an antenatal visit or a discharge summary.
In this way we can, in colloquial terms, 'have our cake and eat it too'. At the same time, CKM ensures tight clinical knowledge governance, yet templates allow for expression of clinician diversity.
Benefits
Archetypes provide a 'glide path' to knowledge-level interoperability of health information. They can:
- Bootstrap new application development – a source of agreed clinical content, avoid re-inventing the wheel for each vendor, organisation or project;
- Provide a forward 'roadmap' for existing applications – supporting gradual transition from proprietary silos to common data representations, perhaps via mapping to common messages as an interim step;
- Support data integration – the means to migrate valuable silos of legacy data to a common, re-usable representation
- Enable data aggregation & comparative analysis – the basis for ensuring 'apples' are 'apples', not 'oranges';
- Simplify messaging – keep message content consistent with EHR content;
- Enable knowledge-based activities eg Clinical Decision Support Systems – consistent & coherent; create once, re-use in all systems.
Power drills, Cardiologists and collaborative consumption
This week I watched Rachel Botsman's TEDxSydney talk: Collaborative Consumption. Rachel's premise is that we're "wired to share", and I particularly liked her illustration at the 10 minute, 30 second mark... ASSUMPTION #1: Most people own a power drill.
ASSUMPTION #2: Most power drills are used for a total of 12-13 minutes in their entire lifetime << seems not unreasonable.
NEED: We actually need a hole, not a drill!
CONCLUSION: Either rent a drill from someone else, or rent yours to everybody else.
WHAT IS THE END GOAL?: Share the resources better!
[ted id=1037]
While visiting Brazil last year , I learned that in São Paulo if you get referred to a Cardiologist, you don't get to choose which one, you just get sent to one. That doesn't sit well with me, especially as a clinician, and I'm pretty careful to whom I entrust my care, or my family's care.
Yet apparently the waiting time is down to trivial time frames. People are actually getting treated. That is significant!
Apparently resources are being used better, simply because of a central booking system and an algorithm matching clinician with patient and location.
When you start to add in some of the benefits from eHealth such as potential shared EHRs, this starts to make more sense. I will still struggle with the lack of choice, but if patients are being seen more efficiently... then maybe it is a good, or even better, thing.
Stop for a moment and consider:
If we want health reform...
If we want more efficient use of resources for our health $$$...
... then we need to think of how to better use Health IT to support the notion of collaborative health consumption - both of resources & information. How can we better match available resources with need? How can we enable consumer choice at the same time?
There's a tension there - I can foresee many issues, but also opportunities.
I have more questions than answers.
Very interested in your opinion.
Is an incremental approach to EHRs enough?
Attending the International Council meetings on the first day of the recent Sydney HL7 meeting, the resounding theme was that of many countries focussed on messages, documents and terminology as the solution for our health IT future; our EHRs; health interoperability. 19 countries presented and 18 repeated this theme. The nineteenth HL7 affiliate, Netherlands, stood out in splendid isolation by declaring an additional focus on the development of clinical content.
Incremental EHRs?
This common message/document/terminology approach to EHRs is largely for historical reasons - safe, solid and incremental innovation; building on what has been proven successful before. It is not unique to health IT. It is not unique to HL7 either - it was just very obvious on the day.
In fact you can see this same phenomena in many places in everyday life - the classic example being the manufacturing of disposable shavers. First a one blade razor, then two blades, then three... But how long can this go on for? Is seven blades a reasonable thing? Eight? Will infinitely more blades make a difference to the shaving outcome or experience? When will blade makes stop and rethink their approach to innovation?
Certainly messages, documents and terminology are approaches that have commenced as often relatively isolated islands of work, had some successes, progressed and are now gradually being drawn together to create opportunities for some interoperability of health information. And don't get me wrong, there are absolutely some successes occurring. However, three questions linger in my mind about this approach:
- Is it enough?
- Is it sustainable?
- Will it achieve interoperable systems?
We all hear the rhetoric that if we can interconnect financial systems, then we can do it for health. We've tried this incremental approach for over 30 years and made significant progress but we definitely haven't cracked it yet.
 Messages
Messages
Paul Roemer used this diagram (right) to illustrate his view of the messaging exchanges in his blog post. I think the image is powerful, imparting both the complexity and chaos that an n-to-n messaging dependency will likely entail. The HIE approach might help, but ultimately a national approach to messaging will result in multiple images like this trying to connect to each other.
This is further complicated by messages often taking up to a year to negotiate between the sender and receiver, or potentially longer to successfully negotiate the national or international standards processes, and even then the resulting 'standard' is often being subjected to individual tweaks and updates at implementation in real-world systems where the 'one-size fits all' message doesn't meet the end-user's requirements.
In Australia the 'standard' pathology HL7 v2.x message is anything but standard with each clinical system vendor having to support multiple slightly different versions of the 'standard'. The big question is whether this is sustainable into the future.
In the US, the clinical content payload for the Direct project is yet to be determined and defined - "The project focuses on the technical standards and services necessary to securely transport content from point A to point B, and does not specify the actual content exchanged." This rings alarm bells for me.
I've been told that at one relatively large hospital system in the US, they require 30 permanent staff just to maintain their messages...! Whoa!!!
Messages and message networks try to be a simple incremental solution to interoperability. But are they really that simple? Are they sustainable? Locally, yes. Regionally, yes probably. Nationally? Internationally???
<My head hurts>
Documents
CDA documents featured highly on the HL7 agenda, with the current emphasis on simple documents, and increasingly we will welcome the inclusion of structured clinical content detail. Currently the content is HL7 v3 templates, but how will that content be standardised and support semantic interoperability?
Werner Ceusters describes semantic interoperability as:
Two information systems are semantically interoperable if and only if each can carry out the tasks for which it was designed using data and information taken from the other as seamlessly as using its own data and information.
Without working towards standardising clinical content we run the risk of our EHRs being little more than a filing cabinet full of unstructured documents that are human readable but not computer processable.
Terminology
We all need terminology, no matter which approach. That is an absolute given.
However the stand-out question that impacts all approaches is how to best 'harness' the terminology...
Interestingly the openEHR Board and the IHTSDO Management Board (SNOMED CT) have been talking about joining forces. An announcement on the openEHR site, in December 2010, states:
"At its October meeting in Toronto, the General Assembly of the IHTSDO received and discussed a proposal, submitted by its Management Board, to support, develop and maintain the IP in openEHR, within a broader framework of IHTSDO governance for clinical content of the electronic health record.
The openEHR Foundation Board has now heard from the IHTSDO Management Board, saying that, whilst the objective of the proposal was considered by the GA to be within the scope of the organisation and that it represented a pressing issue for their governments, it was unable to reach consensus that going forward with openEHR in this way is the right choice, at this time."
This suggests that the IHTSDO Management Board identified significant value in combining the structure of openEHR archetypes with SNOMED, enough to propose a stronger relationship. It will be interesting to see if these discussions continue to progress.
My view - this would be a game-changer. A common approach to using archetypes and SNOMED together is a potentially very powerful semantic combination.
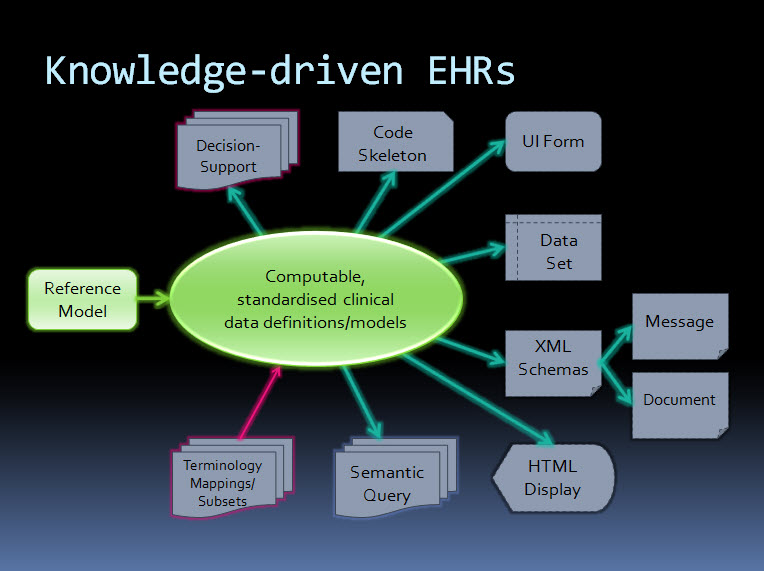
An orthogonal approach - knowledge-driven EHRs
By contrast, the orthogonal approach taken by ISO 13606 & openEHR starts with computable, standardised clinical data definitions at the core - representing the clinical content within an electronic health record. The data definitions, comprising archetypes plus terminology, are the key. Messages and documents are derived from these content specifications and will therefore be internally consistent with the EHR data from which they were generated and if received into an archetype-enabled system can be incorporated, as described by Werner's definition above, as though generated in the receiving system ie semantic interoperability - no data transformation required. The openEHR communities of clinicians, informaticians and engineers are collaborating to agree and standardise these archetypes as a common starting point.
Working from standard content definitions will potentially make the development of documents and messages orders of magnitude simpler. If archetypes have been agreed and published via the CKM collaborative process, then engineers will be able to utilise these as building blocks for the creation of messages and documents for specific use cases, and for a multitude of other technical outputs.
The way forward?
Returning to the multi-blade EHR idea...
When will we stop, regroup and assess the merit of continuing as we are? Who will draw a line in the sand?
Difficult to answer.
Maybe never, maybe no-one.
openEHR/ISO 13606 may not be the right or final answer, but it does provide an alternative and orthogonal approach that has merit and is worth consideration.
Hopefully some of outcomes/proposed discussions from the recent HL7 meeting in Sydney will also contribute to clarifying a way forward.
Perhaps, even yet, we will devise a truly innovative approach to solving the difficulties of developing EHRs.
Adventures of a clinician in HL7!
I've just survived my first HL7 meeting, although amused colleagues tell me that I may not fully recover! ‘Clinician newbie’ to HL7 though I was, for my sins I am becoming increasingly drawn into work within other standards organisations, and my clinical work is no longer with patients but in working with clinicians to develop clinical content models for use in electronic health records. I have some experience of the world of health informatics.
Held relatively nearby in Sydney, it was too good a chance to miss attending an Australian HL7 meeting, and it was an ‘interesting’ experience. The meeting was certainly very casual with a plethora of geeky T-shirts and pony-tails – definitely not the norm at the ISO meetings I’m more familiar with. Some defied this stereotype and still wore their business suits, despite jet-lag and it being a weekend – there are definitely certain individuals that I’ve met over the years who I can only believe must paint the fence in a suit... I particularly remember a certain medical registrar that I worked with many years ago, who always turned up to a resuscitation in Emergency in the middle of the night with a tie perfectly knotted – go figure! But I digress...
I’m told that as the meeting was held outside the US, there was a different flavour of attendee – certainly many from Australia and New Zealand took the opportunity to attend for the first time. I gather many ‘regulars’ didn’t attend and so many of the clinically-related working groups did not meet at all, which was rather disappointing. I spent time in the Patient Care working group and attended the Clinical Interoperability Council. Unfortunately I’m still rather clueless about the remit of the CIC... for clarification in the future perhaps, but clinician-driven approaches to EHR development is a critical way forward, in my opinion.
There was certainly an emphasis on education at this meeting, and it appeared to be very successful with many first-time attendees getting involved, including myself. I attended the Introductory and Advanced tutorials on CDA.
Some highlights:
- Without a doubt the absolute highlight was non-work related - the evening ‘networking reception’ held during a sunset cruise on Sydney Harbour (see the photo above). Rather spectacularly, the organising committee somehow arranged for some rather large yachts to breathtakingly race around us just before sunset. Brilliant!
 Sharing a beer, or three, with Keith Boone. I was chuffed when he blogged that he was coming to meet me! And I’m pleased to report that I seemed to have some impact on him after showing some of our collaborative work happening on the openEHR CKM.
Sharing a beer, or three, with Keith Boone. I was chuffed when he blogged that he was coming to meet me! And I’m pleased to report that I seemed to have some impact on him after showing some of our collaborative work happening on the openEHR CKM.- A refreshing open-mindedness towards our work in openEHR. I particularly like the symmetry – I attended Bob Dolin’s Advanced CDA tutorial, and Bob attended our openEHR sessions! We do have potential to learn from each other.
The outcomes:
I've definitely been encouraged by some of the HL7 meeting outcomes with respect to openEHR. There was definitely a different attitude towards exploring openEHR/HL7 collaboration:
- A DCM feasiblity demonstration project has been proposed - with input from the Patient Care, Models & Methodology and Templates groups.
- Start with archetypes as the base
- Establish adornments that map these to the V3 Ontology (Structured Vocabulary and RIM)
- Create tools that then consume these to produce useful HL7-V3 artifacts (templates, or such)
- An afternoon was spent discussing openEHR & RIMBAA - focussing on the commonalities between openEHR and HL7 RIMBAA implementation issues
- The opportunity to provide tutorials on openEHR within a formal HL7 meeting – the previous attitudes have been more confrontational than collaborative! Which approach will prevail? Rather than how can we learn from each other! The introductory session in the morning was focused on background and clinical knowledge management. The afternoon had a range of speakers with expertise in application of openEHR/ISO 13606 in the HL7 environment
For the future:
- I'd love to have a chance to engage with the Clinical Interoperability Council - to explore how we can collaborate across technical approaches so that at least as clinicians we can ensure that the clinical content in our desktop EHRs is consistently represented, high quality and 'fit for purpose'. The DCM feasibility project outcome will heavily influence if and when this could productively occur.
- As clinicians we have to ensure our access and input to these technical processes, otherwise we won't end up with systems that support us to provide care to our patients. And I challenge the standards bodies to 'demystify' the technical - to remove the technical barriers that prevent grassroots clinician input and restrict participation to those very few who can bridge the world of software engineering with clinical practice.
Other posts from the meeting:
- Rene Spronk: Ringholm - HL7 and openEHR are cooperating (finally)
- Keith Boone (@motorcycle_guy):
- Triplets
- @motocycle_guy: @omowizard An archetype, a DCM and a template walk into an #HL7WGM event, stroll up to the bar ... and the bartender says...
- @omowizard: @motorcycle_guy ...identical triplets I presume! #HL7WGM
- Convergence - regarding templates, detailed clinical models and archetypes
- Triplets